Over 50,000 pre-term births averted during the pandemic, new large-scale analysis shows
1 March 2023
The research, supported by the International COVID-19 Data Alliance and HDR UK, suggests the reduction in pre-term birth rates may be due to less air pollution and improved hygiene practices experienced during the COVID-19 lockdowns.

New results from the International Perinatal Outcomes in the Pandemic (iPOP) Study have been published in the journal Nature Human Behavior. This large, multidisciplinary study of 52 million births from 26 countries found a 3-4% relative reduction in preterm births (defined as birth before 37 weeks gestation) during the first four months of COVID-19 lockdowns.
The researchers noted that the reduction in preterm births during the pandemic was limited to low-income countries. Potential reasons for this decrease may include fewer non-COVID infections (due to improved hygiene practices) and reduced air pollution (due to abrupt reductions in traffic) during the lockdown period. Both infections and air pollution are known to trigger inflammation, which contributes to preterm birth.
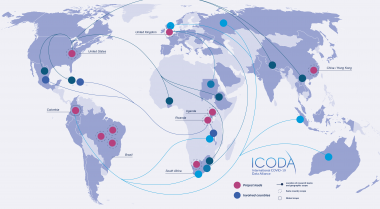
The study was supported by the International COVID-19 Data Alliance (ICODA), an initiative funded by the Bill and Melinda Gates Foundation and Minderoo and convened by Health Data Research (HDR) UK, in addition to support from the HDR UK BREATHE Hub.
In an average year, there are an estimated 14.8 million preterm births worldwide, meaning that even a modest reduction could have a large impact on global birth trends. “We estimate that nearly 50,000 preterm births were averted in the first month of lockdown alone,” say the authors.
Preterm birth and related complications are the leading cause of infant mortality worldwide. While many preterm births start spontaneously, some babies are delivered intentionally early because of emerging pregnancy complications, including stillbirth. In other words, declining rates of preterm births could potentially mask higher rates of stillbirth due to reduced access to care or other factors related to COVID-19 lockdowns.
Among high-income countries (HIC), the iPOP Study did not find a change in stillbirth rates. Conversely, data from Brazil showed an increase in stillbirth rates during the second, third and fourth months of lockdown. One potential cause for the shift in stillbirth rates in some countries may be related to delayed or reduced access to quality healthcare during the early stages of the pandemic.
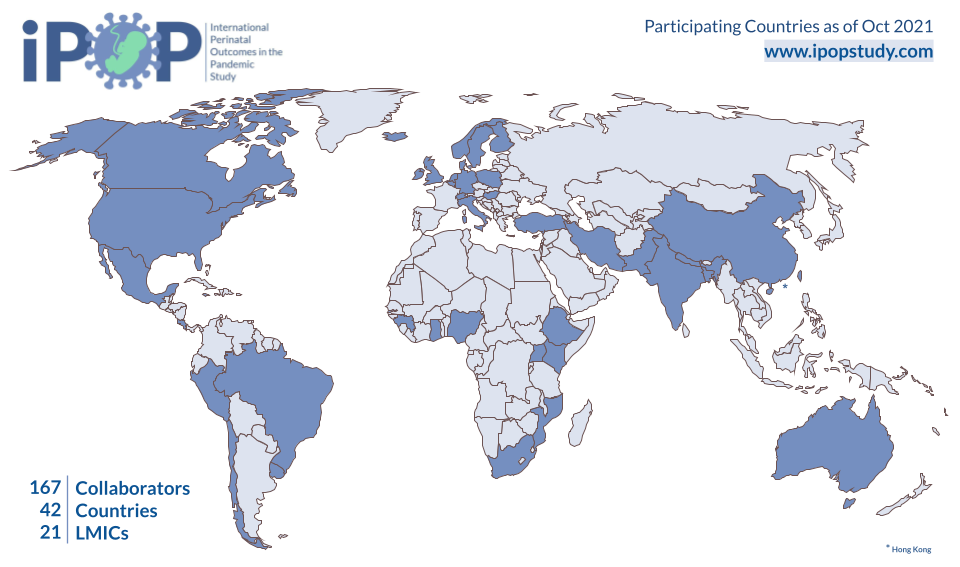
The dataset includes over 52 million births from 26 countries between January 2015 and July 2020. This research represents one of the first large-scale analyses of birth outcomes during the early months of the COVID-19 pandemic. Previous research relied on smaller datasets or on populations within a single socioeconomic, regional or cultural group. The scope and breadth of the iPOP dataset allow researchers an unprecedented look into global birth trends during the shifting pandemic landscape.
“This research represents an incredible partnership between 167 collaborators across 42 different countries,” explains Natalie Rodriguez, Director of Operations, Diversity & Inclusion, THRiVE Discovery Lab at the Children’s Hospital Research Institute of Manitoba & University of Manitoba, Canada.
The iPOP study also includes data from 21 low- and middle-income countries (LMIC). As a result, this research may provide a clearer look into global trends compared to research that solely focuses on a single region or country.
“Collaborative partnerships forged during the iPOP study will continue to strengthen and grow public health research around the globe long after the iPOP results are published,” says Rodriguez.
The study developed at an astonishing speed, particularly given the scope of the collaborative partnerships. “In five months, we went from a tweet to a 100-member consortium,” reports Dr. Azad, who co-founded the study in June 2020.
“The iPOP study united and mobilized public health researchers in a truly unprecedented way,” continues Dr. Azad. “This level of collaboration was grounded in a unified sense of purpose that couldn’t have happened at another period in history. Everyone was eager to do their part to support mothers and babies during a global health crisis.”
Data collected during the iPOP study has far-reaching implications. “This is a legacy dataset,” says Rodriguez. “The scale of data collected during the iPOP study will be utilized for future research projects for years to come.”
Another unique feature of the iPOP study is the role that patients played in the research. “Patients and knowledge users are experts, just like the researchers,” says Dr. Merilee Brockway, one of the original co-leads of the study. To encourage actionable policy and practice recommendations, the iPOP consortium worked closely with partners like the World Health Organization (WHO), the United Nations Population Fund, World Vision and the Public Health Agency of Canada, among others.
More information about the study may be found on the study homepage, including a one-page summary of the study design.