P-NEWS: personalised early warning scores for preventing unplanned critical admissions

This project aims to reduce intensive care admissions by intervening earlier to correct problems before they become critical. They plan to do this by using patient observations and advanced analytics to produce an accurate risk of deterioration for any individual patient.
The Challenge
Unplanned emergency admission to intensive care is associated with poor patient experience, poor outcomes and high resource use. In many cases, there is an opportunity to intervene prior to intensive care admission to correct problems before they become critical or to better understand a patient’s wishes about how they would like to be cared for if they become seriously unwell.
The NHS has implemented a system to detect patients at risk of deterioration – the National Early Warning Score (NEWS). This takes six bedside observations, such as blood pressure and pulse rate, and calculates a number to signify how unwell a patient is. Unfortunately, it has limitations: it is a ‘one size fits all’ regardless of patient type and diagnosis, and it was designed to be computed from static records of patient physiology on wards that use paper charting.
The Solution
At the University Hospitals Bristol NHS Foundation Trust, these observations are now recorded electronically. This enables more information about the patients to be combined with clinician observations and advanced analytics to produce a more accurate risk for any individual patient – so called ‘Personalised-NEWS’ (P-NEWS).
There are over 820,000 sets of electronic observations (e-obs) for around 160,000 patients at the Trust. Using these data, the team will improve on the predictive performance of NEWS, using machine learning to personalise the score based on patient subtypes and exploiting dynamic features extracted from the e-obs time series.
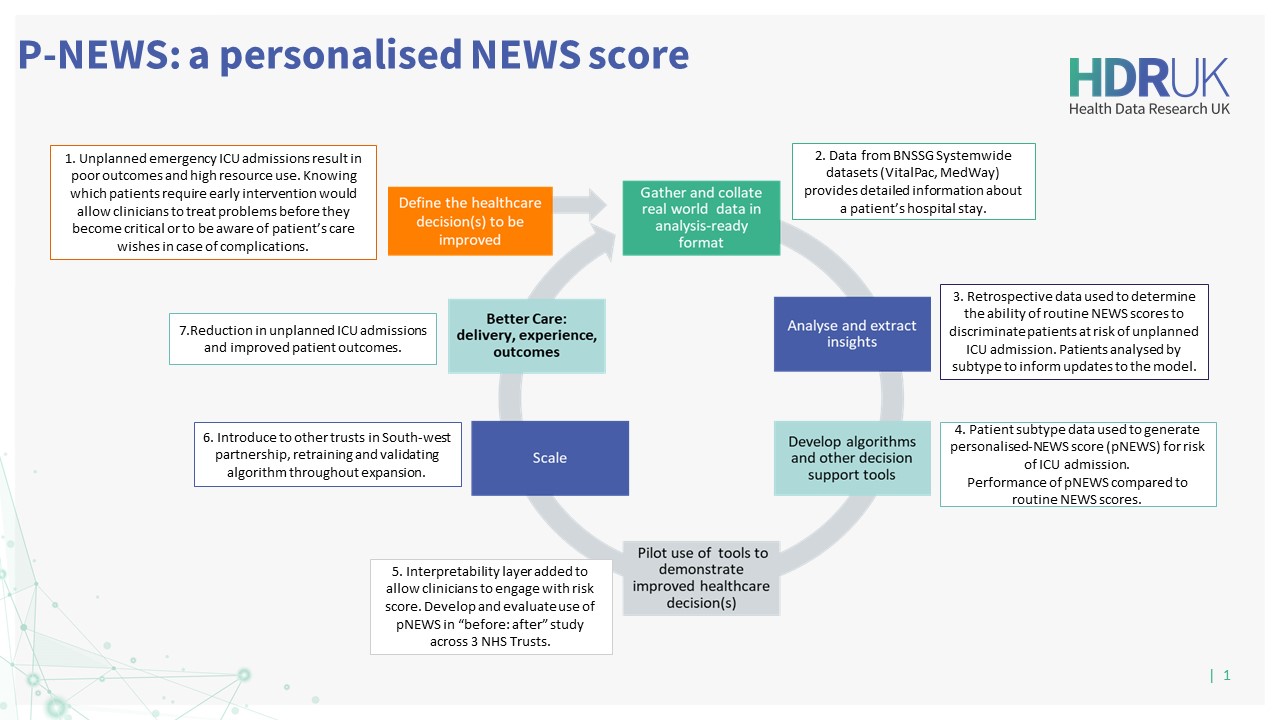
They will perform clustering to determine patient subtypes and then develop predictive models for risk of intensive care unit (ICU) admission for each patient subtype. The resulting risk score – P-NEWS – will be validated in two secondary NHS trusts to produce a generalisable intervention that could be deployed at scale across the NHS. P-NEWS will be implemented and evaluated through a Better Care Loop for unplanned emergency admissions to intensive care.
The Impact and Outcomes
Patients will benefit from an improved hospital experience by ensuring that those requiring an elevated level of care are more reliably identified as early as possible and referred to the appropriate clinical staff to make decisions about their care.
P-NEWS will also produce operational benefits at the system level by reducing the frequency of unplanned emergency admissions to ICU and reducing length of stay in ICU. These changes will allow more efficient resource allocation and have knock-on effects such as reducing the unpredictability in scheduling elective surgeries.
By improving on the timeliness of detection, clinicians using P-NEWS will be able to make earlier treatment decisions that will improve outcomes and may avoid the need for intensive care altogether.
Better Care Loop
Project Team
Dr Chris Bourdeaux, Consultant in Intensive Care Medicine and Chief Clinical Information Officer, University Hospitals Bristol NHS Foundation Trust
Dr Raul Santos-Rodriguez, Senior Lecturer in Data Science and Intelligent Systems, Faulty of Engineering, University of Bristol



